- As a predictor of early death loneliness surpasses even obesity. The following paper, a meta-analysis, concludes that social isolation and loneliness increases risk of mortality of ~30%.
- A universal income could make life alot happier and creative, Alan Watts argues https://www.youtube.com/watch?v=OhvoInEsCI0 (may even be a solution for an increasing global unemployment issue).
- How to manage mild hypertension.
- The is no proven benefit of peer review and tonnes of evidence of the downsides of it. Fraud, repeatablity, slow, biased, luck can be involved, wasteful of scientific time, irrelevant, no quality assurance, inefficient and easily. The perils of Peer Review.
- Free lessons on behavioural medicine
- The so called 'overjustification effect', that a reward can reinforce the belief that a task isnt worth doing. So rewarding children for doing chores or helping out is potentially a bad thing and rewarding yourself for goals an potentially be detrimental.
- How to teach medical students
- that OK GO are back with a new video: https://www.facebook.com/okgo/videos/10153836041340683/
Thursday, 24 November 2016
What did I learn today
Saturday, 19 November 2016
RE: RE: Antibiotic sensitivity overview +tertacycline/doxycycline
Note: Some Strep. pnemoniae are sensitive to tertacyclines, and tetracyclines have modest action action gram negatives such as Neisseria.meningitidis and Haemophilus.influenzae. Tetracycline is good against Clostridia.spp of the anaerobes.
Friday, 18 November 2016
How do I study for this?
Studying in my final year of medicine, there is one question I get asked by the years below me all the time. "how do you study for this? what should I study from, the books, pubmed or the internet?"
Compared to twenty-thirty years ago and with the boom of the internet we have a huge amount of resources at our disposal. And its this huge variety in educational resources makes this question an increasingly common one. Here is my answer:
Disclaimer: First of all, everyone has their own best method, some people learn best from videos, others from quizzes and case studies, this is an important disclaimer when considering study methods.
What is there?:
Textbooks:
The bread and butter of medical study. Often huge, boring and full of what some may consider unnecessary detail. Older doctors will swear by them and the younger doctors may completely avoid them. Use your textbooks as reference! No one has time to read the entire Goodman and Gilmans pharmacology or Kandels textbook of neuroscience. Textbooks are becoming increasingly thicker and thicker and the level of information can terrify first and second year students. When it comes to the fundamentals however, use them! but look for concise or targeted student versions:
Anatomy - Greys anatomy for students
Physiology- Berne and levys physiology
Pharmacology- Rang and Dales
These kind of books for the basic sciences are a must read in their entirety, try and find a smaller concise version for each core subject afterwards. Its in the clinical subjects where you should only use textbooks for reference, Harrison Cecils etc.
Read them, make brief notes, highlight important concepts, bookmark pages, the fundamental textbooks need to look like they have survived a train-wreck after the first couple years of medicine.
moving to the clinical years is where things get tricky...
Wikipedia:
Whenever you google a clinical condition the first post is most likely to be wikipedia post. Hugely informative and structured perfectly with sections for diagnosis, presentation, prognosis and related diseases etc. Take it with a grain of salt. Wikipedia is created by hardworking freelance contributors, many the posts are accurate and uptodate but you never know, they may not be! Until wikipedia has more efficient controls in place, its best used as a quick refresher and definition search tool
Pubmed:
The centre of all that is EBM (eveidence based medicine), you can effectively answer any clinical question here for free. however, its hard work! often you have to search hundreds of articles, and even if you find a nice review, it will probably contain many pages of information that you just arn't ready for yet as a medical student. which brings me to Uptodate
UptoDate:
Requiring a login or at least a registered institution, its not free! However this is the best place hands down to answer any clinical question you may have. The information is reviewed regularly and all the relevant clinical information that is interspersed through articles on pubmed is concentrated here. Again there is the issue of perhaps being a little too advanced for the average medical student. Best used a reference to clinical questions especially patient and disease management questions.
Lectures:
Tedious, time consuming and highly dependant on the skill of the lecturer. We have all sat through a lecture so boring that you struggle to keep your eyes open, it can be a waste of time. On the contrary we have all been to that amazing lecture that kept us on the edge of our seat and full of curiosity at the end. Sometimes I feel I learn more from certain lectures than I ever could in a day reading through the relevant textbook. As much as we moan and and groan about them, lectures are important! attend them, drink coffee, and make notes! lectures will form the backbone of your study and are an important place to cement the core concepts you will need to study in revision. The medical exams are often about what you were lectured on remember.
Clincal cases and question books/sites:
Use these after you have studied, prior to exams. The best way to really test if you really know a subject is to test yourself. Often through testing yourself you find the holes in your knowledge base. it really works! Clinical case books are excellent, a little tedious but are probably the best way to test yourself in a way that will prove to be useful when you start work as a doctor (that special way of thinking when you approach a patient). Multiple choice question books and similar quiz books have now been surpassed by websites with endless question banks. The BMJ on examination site (which I use regularly) is just fantastic. One of my colleagues swears by the Firecracker app, where he answers about 50 quick questions a day on the metro/underground on the way and back from university. Unfortunately there is a catch, these questions banks can be incredibly expensive, so maybe its best to use these resources only before the big exams such as finals or end of phases.
Senior and classmates notes:
Forget it, the source isnt always reliable and most of the learning is in producing the notes yourself. One of my colleagues makes a killing selling his anatomy notes to first years, perhaps a good buisness solution, dont fall for it. On the plus side, notes may be targeted to an exam well and help when you have missed lectures. My advice, avoid if possible.
Group sessions:
Moving a bit away from the topic of resources, group studying is a real preference for some people. I think I will address the debate 'group vs solo studying' in another post. It depends a lot of the group itself and the study method, tackling clinical cases together is a good method.
Youtube:
What a resource, there are hundreds of videos on youtube and many of them are fantastic. I mentioned in a previous post Paul Bolin lectures and how they are brilliant for students preparing for the USMLE. Youtube is probably the best place for people interested in surgery and procedural medicine. Intubation, inserting catheters, chest drains and surgical approaches its all there (although can take some searching to find decent videos and in the correct language). Its incredibly difficult to learn a procedure from reading a book or passage, they are best learnt visually in a step by step matter, or better yet on the ward!!
The ward:
A must for all students. Spending time on the wards presents potential learning opportunities in areas which are favoured by in examinations, particularly practical assessments. Remember that medical school is a precursor for life as a doctor and thus, adequate exposure is necessary to assimilate the abilities expected of new doctor when they start. Although tempting to spend less time on the wards, especially near exams, try not to skip these session. Take a pen and note pad, note down everything you learn or new drug/disease/concept you hear. Try and take at least one history every time you are on the ward.
Medical blogs (like me :)):
There are some incredible medical blogs out there, life in the fast lane and emergency anatomy to name a couple that I usually use. It can be difficult to keep track of the variety in posts and to stay on track when studying a particular subject. You have to be careful with the accuracy of the information and sometimes it best to use the references in the post and read the original material before even reading the main post. I kind of feel that blogs are actually best for gaining an insight into the world of medicine, for opinions on the latest research and methods and for all that humanitarian stuff that forms much more of medicine than most of us are aware about. Patient care and professionalism are fundamental to a great doctor, it can be hard to find a good understanding about some of these issues from textbooks, blogs are invaluable! (not many textbooks will have a part about how to study like this will they ha).
Twitter:
There is an amazing movement happening in medical education at the moment, the hashtag or FOAMed movement. Hashtags like #FOAMed and #MEDed are attached to various things from the internet (videos, blogs, websites) to form this huge collection of medical education resources. More specific hashtags can be used to focus on the subject at hand #FOAMcc for crtical care for example or even summarize the findings from important conferences like #AHA16. Its a wonderful movement and its keeping medicine uptodate almost instantaneously and completely for free. Watch this space!
Ok I have rambled on a bit now and my lunch break is ending. Here is my best answer to the question above:
Attend lectures, make notes and read through them briefly that same day. Use the lectures to form a kind of back bone of core topics. Use the text book to cover these core topics by subject. And use the entire textbooks when addressing core fundamentals like anatomy and physiology.
When you start clinical modules, use smaller review books with a more concise approach (I'm thinking Kumar and clarks vs Harrisons for example or Surgical talks vs Sabistons surgery). Whenever you have a clinical question use Uptodate and Pubmed. If you feel you need to understand something better use the fundamental textbooks. Try and explore the topics with twitter and blogs. When you are close to exams use clinical case books and online question banks, referring to the textbooks when you find a hole in your knowledge.
NOTEs:
_The Eisenhower box to time management, works for studying too:
Remember you don't have to study everything in order, spaced repetition is the better way of learning in the long term.
Any questions feel free to comment and Ill get back to you, gotta runn..
Disclaimer: First of all, everyone has their own best method, some people learn best from videos, others from quizzes and case studies, this is an important disclaimer when considering study methods.
What is there?:
- Fundamental textbooks
- Wikipedia
- Pubmed
- Uptodate
- Lectures and lecture notes
- Clinical case and question books/sites
- Revision books
- Senior and classmate notes
- Group sessions
- Youtube
- The ward
- medical blogs
- FOAMed/MEDed and twitter
(SKIP TO SUMMARY/ANSWER AT THE END IF YOU LIKE)
Textbooks:
The bread and butter of medical study. Often huge, boring and full of what some may consider unnecessary detail. Older doctors will swear by them and the younger doctors may completely avoid them. Use your textbooks as reference! No one has time to read the entire Goodman and Gilmans pharmacology or Kandels textbook of neuroscience. Textbooks are becoming increasingly thicker and thicker and the level of information can terrify first and second year students. When it comes to the fundamentals however, use them! but look for concise or targeted student versions:
Anatomy - Greys anatomy for students
Physiology- Berne and levys physiology
Pharmacology- Rang and Dales
These kind of books for the basic sciences are a must read in their entirety, try and find a smaller concise version for each core subject afterwards. Its in the clinical subjects where you should only use textbooks for reference, Harrison Cecils etc.
Read them, make brief notes, highlight important concepts, bookmark pages, the fundamental textbooks need to look like they have survived a train-wreck after the first couple years of medicine.
moving to the clinical years is where things get tricky...
Wikipedia:
Whenever you google a clinical condition the first post is most likely to be wikipedia post. Hugely informative and structured perfectly with sections for diagnosis, presentation, prognosis and related diseases etc. Take it with a grain of salt. Wikipedia is created by hardworking freelance contributors, many the posts are accurate and uptodate but you never know, they may not be! Until wikipedia has more efficient controls in place, its best used as a quick refresher and definition search tool
Pubmed:
The centre of all that is EBM (eveidence based medicine), you can effectively answer any clinical question here for free. however, its hard work! often you have to search hundreds of articles, and even if you find a nice review, it will probably contain many pages of information that you just arn't ready for yet as a medical student. which brings me to Uptodate
UptoDate:
Requiring a login or at least a registered institution, its not free! However this is the best place hands down to answer any clinical question you may have. The information is reviewed regularly and all the relevant clinical information that is interspersed through articles on pubmed is concentrated here. Again there is the issue of perhaps being a little too advanced for the average medical student. Best used a reference to clinical questions especially patient and disease management questions.
Lectures:
Tedious, time consuming and highly dependant on the skill of the lecturer. We have all sat through a lecture so boring that you struggle to keep your eyes open, it can be a waste of time. On the contrary we have all been to that amazing lecture that kept us on the edge of our seat and full of curiosity at the end. Sometimes I feel I learn more from certain lectures than I ever could in a day reading through the relevant textbook. As much as we moan and and groan about them, lectures are important! attend them, drink coffee, and make notes! lectures will form the backbone of your study and are an important place to cement the core concepts you will need to study in revision. The medical exams are often about what you were lectured on remember.
Clincal cases and question books/sites:
Use these after you have studied, prior to exams. The best way to really test if you really know a subject is to test yourself. Often through testing yourself you find the holes in your knowledge base. it really works! Clinical case books are excellent, a little tedious but are probably the best way to test yourself in a way that will prove to be useful when you start work as a doctor (that special way of thinking when you approach a patient). Multiple choice question books and similar quiz books have now been surpassed by websites with endless question banks. The BMJ on examination site (which I use regularly) is just fantastic. One of my colleagues swears by the Firecracker app, where he answers about 50 quick questions a day on the metro/underground on the way and back from university. Unfortunately there is a catch, these questions banks can be incredibly expensive, so maybe its best to use these resources only before the big exams such as finals or end of phases.
Senior and classmates notes:
Forget it, the source isnt always reliable and most of the learning is in producing the notes yourself. One of my colleagues makes a killing selling his anatomy notes to first years, perhaps a good buisness solution, dont fall for it. On the plus side, notes may be targeted to an exam well and help when you have missed lectures. My advice, avoid if possible.
Group sessions:
Moving a bit away from the topic of resources, group studying is a real preference for some people. I think I will address the debate 'group vs solo studying' in another post. It depends a lot of the group itself and the study method, tackling clinical cases together is a good method.
Youtube:
What a resource, there are hundreds of videos on youtube and many of them are fantastic. I mentioned in a previous post Paul Bolin lectures and how they are brilliant for students preparing for the USMLE. Youtube is probably the best place for people interested in surgery and procedural medicine. Intubation, inserting catheters, chest drains and surgical approaches its all there (although can take some searching to find decent videos and in the correct language). Its incredibly difficult to learn a procedure from reading a book or passage, they are best learnt visually in a step by step matter, or better yet on the ward!!
The ward:
A must for all students. Spending time on the wards presents potential learning opportunities in areas which are favoured by in examinations, particularly practical assessments. Remember that medical school is a precursor for life as a doctor and thus, adequate exposure is necessary to assimilate the abilities expected of new doctor when they start. Although tempting to spend less time on the wards, especially near exams, try not to skip these session. Take a pen and note pad, note down everything you learn or new drug/disease/concept you hear. Try and take at least one history every time you are on the ward.
Medical blogs (like me :)):
There are some incredible medical blogs out there, life in the fast lane and emergency anatomy to name a couple that I usually use. It can be difficult to keep track of the variety in posts and to stay on track when studying a particular subject. You have to be careful with the accuracy of the information and sometimes it best to use the references in the post and read the original material before even reading the main post. I kind of feel that blogs are actually best for gaining an insight into the world of medicine, for opinions on the latest research and methods and for all that humanitarian stuff that forms much more of medicine than most of us are aware about. Patient care and professionalism are fundamental to a great doctor, it can be hard to find a good understanding about some of these issues from textbooks, blogs are invaluable! (not many textbooks will have a part about how to study like this will they ha).
Twitter:
There is an amazing movement happening in medical education at the moment, the hashtag or FOAMed movement. Hashtags like #FOAMed and #MEDed are attached to various things from the internet (videos, blogs, websites) to form this huge collection of medical education resources. More specific hashtags can be used to focus on the subject at hand #FOAMcc for crtical care for example or even summarize the findings from important conferences like #AHA16. Its a wonderful movement and its keeping medicine uptodate almost instantaneously and completely for free. Watch this space!
Ok I have rambled on a bit now and my lunch break is ending. Here is my best answer to the question above:
Attend lectures, make notes and read through them briefly that same day. Use the lectures to form a kind of back bone of core topics. Use the text book to cover these core topics by subject. And use the entire textbooks when addressing core fundamentals like anatomy and physiology.
When you start clinical modules, use smaller review books with a more concise approach (I'm thinking Kumar and clarks vs Harrisons for example or Surgical talks vs Sabistons surgery). Whenever you have a clinical question use Uptodate and Pubmed. If you feel you need to understand something better use the fundamental textbooks. Try and explore the topics with twitter and blogs. When you are close to exams use clinical case books and online question banks, referring to the textbooks when you find a hole in your knowledge.
NOTEs:
_The Eisenhower box to time management, works for studying too:
Remember you don't have to study everything in order, spaced repetition is the better way of learning in the long term.
Any questions feel free to comment and Ill get back to you, gotta runn..
Wednesday, 16 November 2016
RE: Antibiotic sensitivity overview
Modified version of this great post by Dr Michael Shamoon on CORE-EM. I added the orange box for macrolides and includes Clarithromycin, Azithromycin and Erythromycin. (Telithrmycin also has the same sensitivties).
Saturday, 12 November 2016
Forensic Medicine: Death
As a doctor you will inevitably have to deal with death and dying. Its hard and emotionally testing but you have to know what to do. There is a chance that you will be called to certify a death and you may have to make a decision about whether an autopsy is needed. I hope to cover everything about death in this post. disclaimer: I attend an international medical school so the laws may be different in different countries, most of the laws described here fit English and Italian law, I have tried to be as general as possible so to cover most countries.
First of all how does one certify a death and how can you be sure that someone is in fact dead?
The respiratory, cardiovascular and neurological systems are regarded to be essential for life. therefore most assessments of life will address these systems.
When the authorities come to you for a death certification, what they need is a proof of death, they don't need you to determine the cause of death. Usually there will be an ECG at hand and you will certify death by verified lack of cardiac activity (20min continuous ECG). If there is no ECG, then you will have to determine death based on post-mortal phenoma and other physical signs.
There is anyway a mandatory 24hour period of observation of the body (usually in the morgue) just to make sure the body is in fact dead. the observation is mandatory except for putrified bodies (rotting bodies) or with decapitated bodies.
In the UK you can certify death by fulfiling the following criteria:
A couple of examples:
Stab wound - massive hemorrhage - cardiac arrest
Abdominal aortic aneurysm - anuerysm rupture - cardiac arrest
(dont use an abbreviations when filling out this form).
There is an area whee you state comorbidities that may have contributed to the death and a separate area to fill in regarding traumatic deaths (was the death a suicide, homicide or accident). after filing the in the form you simply sign it and state your registration number.
The aim of the MCCD is to monitor deaths in the country, and still quite often we don't know what caused some deaths. For example a patient arrives in ER and dies shortly after or a patient with a history of heart disease dies at the GP practice. You have to pay attention when filling in this form, you should fill in the form with "scientific knowledge and good conscious" as the Italians put it.
a physician should fill in this form only is he or she feels relatively confident about the cause of death (you can never be 100% sure). Any cause of death can be put on the form, if the cause of death is not filled in or the form not submitted then an autopsy will be requested by the national health system (NHS) (hospitals themselves can also request an autopsy). Never feel forced to fill in the form. With autopsies the system feels safer.
If a normal national health autopsy is conducted and suspicious lesions are found for example a neck hematoma, then the autopsy is automatically stopped and referred over to the judicial system. Before a judicial autopsy no one can touch the body (no tampering). There is sometimes are threats to pathologists dealing with a body from gang members.
When a person dies the family will need more
support than ever. 60-70% complaints to doctors regarding life-death issues are due to the family not being given enough
attention and feeling like they were not appropriately listened to. After a death, sit down
and talk to the relatives. There usually is a bereavement team at the hospital you can contact, who will liaise with the family.
First of all how does one certify a death and how can you be sure that someone is in fact dead?
The respiratory, cardiovascular and neurological systems are regarded to be essential for life. therefore most assessments of life will address these systems.
When the authorities come to you for a death certification, what they need is a proof of death, they don't need you to determine the cause of death. Usually there will be an ECG at hand and you will certify death by verified lack of cardiac activity (20min continuous ECG). If there is no ECG, then you will have to determine death based on post-mortal phenoma and other physical signs.
There is anyway a mandatory 24hour period of observation of the body (usually in the morgue) just to make sure the body is in fact dead. the observation is mandatory except for putrified bodies (rotting bodies) or with decapitated bodies.
In the UK you can certify death by fulfiling the following criteria:
- No palpable pulses.
- No heart sounds on auscultation (or asystole on ECG).
- No reaction to painful stimuli
- No breath sounds on auscultation and no observed respiratory effort.
- Pupils dilated and not reactive to light.
Its important to assess without any unnecessary delay and ensure accurate documentation in the patient notes with your assessment and the time of death.
In order to bury a body the national mortuary regulation requires a complete MCCD (medical certificate of cause of death form) with a cause of death. This makes determining the cause of death more important than certifying death as the body cannot be buried without it. The form is used for statistical purposes. The form has three spaces for the cause of death; a final cause of death, an immediate cause of death and an initial cause of death. Its not easy to state what the actual causes and potential chain reaction to death is. Frequently the final cause of death is cardiac arrest or respiratory arrest, but what caused it? A couple of examples:
Stab wound - massive hemorrhage - cardiac arrest
Abdominal aortic aneurysm - anuerysm rupture - cardiac arrest
(dont use an abbreviations when filling out this form).
There is an area whee you state comorbidities that may have contributed to the death and a separate area to fill in regarding traumatic deaths (was the death a suicide, homicide or accident). after filing the in the form you simply sign it and state your registration number.
The aim of the MCCD is to monitor deaths in the country, and still quite often we don't know what caused some deaths. For example a patient arrives in ER and dies shortly after or a patient with a history of heart disease dies at the GP practice. You have to pay attention when filling in this form, you should fill in the form with "scientific knowledge and good conscious" as the Italians put it.
a physician should fill in this form only is he or she feels relatively confident about the cause of death (you can never be 100% sure). Any cause of death can be put on the form, if the cause of death is not filled in or the form not submitted then an autopsy will be requested by the national health system (NHS) (hospitals themselves can also request an autopsy). Never feel forced to fill in the form. With autopsies the system feels safer.
If a normal national health autopsy is conducted and suspicious lesions are found for example a neck hematoma, then the autopsy is automatically stopped and referred over to the judicial system. Before a judicial autopsy no one can touch the body (no tampering). There is sometimes are threats to pathologists dealing with a body from gang members.
Its important to note that the families have no say in what happens to the dead body,
dead bodies do not belong to the family. Although ethical and morally its good
to inform the family about what is happening to the body of course.
Just to highlight, if you are not sure about the cause of death do not sign the form!
There are two laws that protect the dead a first law
protecting the dead against maiming and a second law basically saying that family's have no
say in what happens to the body. Many religions don’t want the body tampered with and this
clashes with the law, the law needs to be respected.
Judicially speaking, a dead body is not a person and therefore
loses the rights of a person. There are many controversies and questions
related to privacy, however the answer usually swings to the fact that dead bodies have no rights like living people.
Every year in Milan 2-3 bodies and in Italy over 1000 unidentified bodies are discovered and
buried without a name. Some places tried to provide a facility where you could put
a picture online of the cadaver in hope of an identity such as the UK missing persons
bureau. Although these can clash with some authorities over privacy issues.
Pathological phenoma following death
These phenoma can be used to identify a person, the time of
death and sometimes even the cause.
After immediate death there is an early post mortum period, then after the decomposition period and finally after that taphonomic factors.
The early post mortum period is what forensic pathologists
and doctors certifying death will mostly be dealing with. You may even get a call
to certify death when the body is already full of worms, but a doctor is still needed
to certify death even in this case.
Three phenoma are seen during the early postmortum period
- Algor mortis (cooling)
- Rigor mortis (rigidity)
- Livor mortis (a hydrostatic phenoma)
Algor mortis (not Al Gore mortis)
Algor mortis starts as soon as the vital activity of the
body stops. We cannot see with the naked eye the metabolic changes on a cellular
level but you can feel and measure the temperature. The body will start at
around 37 degrees on death and will slowly reach the temperature of the surrounding
environment. Never trust if a body just feels cold, always use an objective
measured reading. Depending on the
reference textbook you use, Below 34 degrees is considered not compatible with life. Use an
internal measure of temperature, for example the mouth or rectum (or even
tympanic temperature, see below). The time from
death is linked to the temperature but depends on many variables.
You may be asked if the death was recent or not. You can try
and correlate the environment with the temperature you record, there are in fact
many equations that can be used to estimate the time of death but even the best
of these will give you a result with plus or minus 2 hours minimum from time of death (plus or
minus 4 hours is probably a better considerate). Many of these equations insist on rectal temperature
and hence the error because the
rectal temperature ha a large plateau in which it does not alter, it takes a
while to change.
Ear temperature is much more representative of cooling, the
speed and for how long for. This is because the variables change less in the
head (no difference in body fat surrounding for example). Often many doctors
with take the temperature with the back of the hand, never do that! use a
thermometer!
Rigor mortis
The physiology of rigor mortis is well
understood. The lack of ATP production after death causes ATP to eventually run
out and the actin-myosin contractile unit of muscles to be locked in place (the
myosin heads cannot detach without ATP). The onset takes a little while, while
there is still ATP in the muscle. Eventually the muscle becomes locked in place
and it is a very strong contraction. I read about pathologists forcing the
joints (breaking the joints) in order to get arms or limbs straight. It tends to start at the head and extend down
to the feet and it devolves in the same way from head to feet. It can even take a
few days to resolve in some cases.
Livor mortis
Livor mortis sets in after a few hours. It is quite simply
the pooling blood in the body due to gravity. Slowly as time goes by, the
endothelium collapses and the blood infiltrates the tissues. The pooling of
blood will cause discoloration of the tissues, and you will see pink purple
areas on the skin. If the cadaver was on it's back, the lower part of the body
will be pink and the compressed areas of contact will be white. A handy test is
if you compress the pink area with your finger, if the death was less than
6-10 hours ago then the blood will move away on finger compression (become white). If you were to
roll the body less than 6-10 hours after
death then the pink areas would move, if the death was greater than 6-10 hours
ago then the pink areas will stay pink .
Time frames
First considering algor mortis there are four stages after
death with related time periods
Algor mortis:
0-3hours Plateau phase (no change in temp)
6-8hours Fast cooling stage (most accurate for determining
time of death)
10-12hours Final plateau phase
11-30hours End of cooling.
Rigor mortis depending on the textbook tends to begin at
around the 3hours-12hours mark, with the highest intensity of contractions between 12 and 48hours, resolution is around the 72hours mark.
Livor mortis has an onset around the 2hour mark with the
highest intensity of discoloration at the 12hour mark, at 10hours-12hours the
blood can still migrate at the 48-72hour mark it becomes fixed.
(Note that compression areas will be white and hanging limbs
will be pink, consider gravity).
Transformative processes
When you are asked to certify a dead body you have to know
what to expect. If the death happened a long time ago you will see the so
called transformative processes. When these processes kick in you need to be
aware that its impossible to determine the time of death. The onset and time
frames are incredibly variable and depends on many variables and environmental
factors.
Transformative processs can be either destructive or
conservative.
Destructive:
Autolysis
Putrefaction
Maceration
Conservative:
Mummification
Adipocere
Corification
Mummification is caused by the loss of water from the soft
tissues, and can preserve the tissues for a very long time. In theory if you
rehydrate the tissue you will see the same tissue as before. True mummification
is very rare.
Adipocere usually occurs when the body is left in water, the
tissue becomes a weird creamy soft texture and then sets after a while to an incredibly
rock hard shell.
Damp bodies may not putrefy and can undergo so called wet mummification where all the cells are lost and just the fibrous collagen based skeleton of the tissues remains, it appears very similar to mummification with
brown appearance.
Criminal cases look at the exterior limits of these
processes. It can be hard to not lose body parts when these processes kick in
when you are collecting the body.
Putrefaction is the main transformative
process for dead bodies at our latitude. Putrefaction is decomposition of
the body and causes a marble like green discoloration to the body (green due to hemoglobin catabolism), usually the processes start in the lower right quadrant of the
body (this is because the cecum contains the highest concentration of bacteria
in the GI tract). There is also bloating due to the gases produced. Eventually everything
breaks down and turns to water. When you come across a putrefied decomposed
body this is one of the rare scenarios where on the MCCD you can write the
cause of death as indeterminate.
Many factors affect these processes: temperature, wind,
season, soil pH, moisture content of soil, morphological characteristics, patient
age, cause of death, laceration or discontinuations of the skin.
Thursday, 10 November 2016
"The Solution to Pollution is Dilution"
The in the title quote was originally used in environmental and industrial post-WW2 industries to explain how dumping of waste and chemicals would ok as long as they were sufficiently diluted. In other words, toxins are less toxic in lower concentrations. One of the orthopedic consultants today quoted the same quote in regards to wound management and I got a flashback to those high school geography lessons, but he has a point!
"The Solution To Pollution Is Dilution"
Quite simply in the wound management the more you clean a wound the cleaner it will be. Each wash will wash away some of the bacteria and dirty material. So when cleaning a wound with saline or other sterile liquids remember this! Its a simple concept, but very effective.
Dunning-Kruger Effect, Fake-It-To-Become-It, All trumped out.
So I just found out that Mr Trump will be the next president
of the USA (post written yesterday morning). It’s clear by my Twitter and Facebook feeds that the rest of the
world (particularly Europe) are just as surprised as me. Trump has never failed
to surprise us, from the very point where he decided to run we laughed. After
becoming the republican candidate for presidency we still shook it off and
thought there was no chance he’d be president and now look at how our jaws have
dropped. The eight year old I'm babysitting at the moment genuinely asked me
“does this mean there is going to be a world war 3?” I hope not little guy, I
hope not. One of my favourite analyses of President Trumps (wow that’s really a
thing) electoral run is the so called Dunning-Kruger effect.
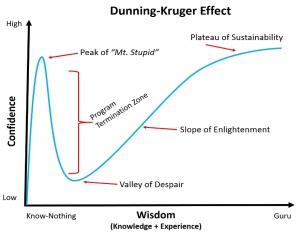
The Dunning-Kruger effect is an interesting cognitive bias
where people who an incompetent are unaware of their own incompetence (top of mount stupid) and people who have high ability may underestimate their own competence. Charles Darwin summarised it well when he said "Ignorance more frequently begets confidence than does knowledge".
The effect seems to be on the rise and this seems to be due
to people being ‘more actively misinformed’. Information is everywhere, and
anyone can write a blog or post about anything (*cough*my own blog*cough*),
encouraging the spread of misinformation. There is really no filter on the
internet. Although, it can be actually quite comforting to think that everyone
is just winging it (writes Oliver Burkman), this is a dangerous place to
be, especially in medicine! Fortunately many medics will find themselves at the
opposite end of the spectrum, in a position where they are overwhelmed by the
shear amount of knowledge and expertise they will need in the future. One way
to approach this is the fake-it-to-become-it approach as popularized in thisTED talk by Amy Cuddy. It works by throwing yourself in the deep end and
working step by step towards the end goal acting as if you were already there
(not without staying humble and keeping that fear of inadequacy of course).
I guess to close this post what I want to point out is that
you can now understand how some politicians seem so certain about everything
while infact knowing nothing (because they in fact know nothing). And one
should assess their own position on the Dunning-Kruger curve from time to time,
by taking a step back, assessing one’s own knowledge objectively and paying
attention to critism carefully.
PS: in reply to the eight year old, I found this interestingbreakdown of how world war three might actually happen by Tobias Stone:
Brexit in the UK causes Italy or France to have a similar referendum. Le Pen wins an election in France. Europe now has a fractured EU. The EU, for all its many awful faults, has prevented a war in Europe for longer than ever before. The EU is also a major force in suppressing Putin’s military ambitions. European sanctions on Russia really hit the economy, and helped temper Russia’s attacks on Ukraine (there is a reason bad guys always want a weaker European Union). Trump wins in the US. Trump becomes isolationist, which weakens NATO. He has already said he would not automatically honourNATO commitments in the face of a Russian attack on the Baltics.With a fractured EU, and weakened NATO, Putin, facing an ongoing economic and social crisis in Russia, needs another foreign distraction around which to rally his people. He funds far right anti-EU activists in Latvia, who then create a reason for an uprising of the Russian Latvians in the East of the country (the EU border with Russia). Russia sends ‘peace keeping forces’ and ‘aid lorries’ into Latvia, as it did in Georgia, and in Ukraine. He annexes Eastern Latvia as he did Eastern Ukraine (Crimea has the same population as Latvia, by the way).A divided Europe, with the leaders of France, Hungary, Poland, Slovakia, and others now pro-Russia, anti-EU, and funded by Putin, overrule calls for sanctions or a military response. NATO is slow to respond: Trump does not want America to be involved, and a large part of Europe is indifferent or blocking any action. Russia, seeing no real resistance to their actions, move further into Latvia, and then into Eastern Estonia and Lithuania. The Baltic States declare war on Russia and start to retaliate, as they have now been invaded so have no choice. Half of Europe sides with them, a few countries remain neutral, and a few side with Russia. Where does Turkey stand on this? How does ISIS respond to a new war in Europe? Who uses a nuclear weapon first?
Tuesday, 8 November 2016
Forensic medicine: Gun Shot Wounds
Depending on where you are working, gun shot wounds (GSWs) may be a rarity or so common that almost everyday you will see a patient with a GSW in the emergency room. GSWs generally have a bad prognosis with a high incidence of gangrene and anaerobic infection. On top of that there is likely to be a criminal investigation regarding the shooting, so knowledge of how to describe a lesion and preserve evidence is incredibly important.
When talking about GSWs you first need to consider the
construction of the bullet and the mechanics of gunfire. Projectiles are most often
made of lead and may be jacketed or not, the jacket is often made of an alloy
like brass (copper and zinc alloy). Here in Italy, unjacketed projectiles are
illegal.
The bullet contains the projectile, jacket and a small amount
of gunpowder which produces the explosion behind which propels the projectile. The gunpowder usually contains the following
chemicals; Barium, Antimony and Lead. These chemicals are what forensics
pathologists look for when they look for evidence, they can sometimes even type the gun with knowledge of the chemical ratio.
On pressing the trigger there is a small explosion and most
of the gunpowder is burnt to produce gas, however some powder will not burn and
be fired along with the projectile.
So when the bullet exits the muzzle of the gun, gas and
small fragments of unburnt powder also
exits the gun like a kind of small pepper spray, there is also residue and
grease from the barrel that is fired along with everything else.
A shotgun bullet is slightly different in that the
projectile is actually a collection on small pellets (the shot) as the pellets
leave the barrel of the gun they spread out so a GSW from a close range shotgun
shot (it forms a large hole) is different to a long range shotgun shot (many small holes).
Bullets may penetrate the body and may exit or stop within
the body. They can ricochet off bone and some are actually made to bounce more
in the body cavities (nasty). The bullet entry hole is usually much bigger than the
actual bullet because as the bullet travels through the air it spins and
oscillates (again some are designed to do this more, for more damage). It can
sometimes be very difficult to tell the difference between the entrance and
exit wound because of this. Bullets may even break and leave multiple exit
wounds from a single a entry point or multiple entries. Usually an entrance
wound is a round discontinuation with no loss of tissue. The residues from the
gun will be on the skin surface around the entrance wound. Its important to use
tape or a stub to collect the residue from the skin surface. In fact you should
keep anything used to clean the wound and the victims clothes as well as they
will contain very important residue.
There are four things you can see with a GSW and it depends
on the distance of the victim from the gun.
- Entry/exit wound
- Tattooing
- Smoke stains
- Burns.
At long distance there will be only the entry and exit
wounds from the bullet. As the victim is closer to the attacker tattooing can
be seen caused by small pieces of unburnt gunpowder that produce small black
spots (penetrating skin) or red spots (excoriations).
At even closer range the smoke from the gun can produce
smoke stains on the skin, colouring the skin around the entry wound black. At
even closer range than this the flame from the gunshot can burn the skin.
All these residues are collected and mapped and compared
often with shooting experiments to determine firing range and gun type (each
gun has its own distinct pattern of residue spread).
If the gun is fired at point blank on contact with the skin,
a so called contact wound is produced. This is often stellate in shape, the
flaps are caused by the pressure of air as it escapes around the gun, it can
look like a blunt force injury so be careful in your description.
If the bullet penetrates a flat bone it can be easy to spot
the entry and exit side from bevelling of the bone edge (the bone will be
bevelled on the exit side of the bone and diameter of the hole as the entry
side has a smaller diameter to the exit side. Exit wounds can be very messy and
may sometimes look like a blunt force injury, sometimes if the victim is
against a surface where the bullet exits eg. A wall, material from the wall
behind can be found in the wound.
In terms of treatment, GSWs must be treated with thorough debridement and delayed primary suture in the same way as battle injuries (future post). It must never be closed straight away! The debridement should be extra thorough taking extra care to remove fragments of clothing and soil from the wound.
Clinically you can divide GSWs into low velocity and high velocity injuries. Low velocity injuries can cause little soft tissue damage as long as they remain stable (remember that oscillation and cartwheeling of the bullet will cause more damage). High velocity injuries act like a small explosion and many tissue planes are separated providing easy access for infections. There is often foreign material in the wound further enhancing chance of infection.
Monday, 7 November 2016
Forensic Pathology
Forensic pathology regards the diagnosis of when a lesion occurred and how it occurred. All physicians will have to deal with violence and trauma at
some point. It is important you can describe a lesion well and accurately as your report may be used as evidence in a court case. You should be able to diagnose a lesion, age it, describe it and know
what to do to preserve evidence.
There is a branch called humanitarian forensic medicine, for
example proving migrants underwent torture in their home country. For these migrants, the evidence
you present may determine whether they will be allowed political
exile or not. Your report is the only piece of paper that will be able to support the evidence
of ill treatment or torture when presented to regional councils and police.
In humanitarian forensic medicine you may also be needed to age unaccompanied minors of undetermined age. For example migrants
without any documents, is the migrant above 18 years age? it could make
all the difference. Police can refuse territory to migrants over 18yrs. You need
to know what to do to verify age.
Forensic pathology starts with a physical exam. You need to
assess the whole body (you also need to listen to the patient, don’t forget!).
If you don’t document a lesion or ‘crime’ and the victim doesn’t talk, then any
evidence of the ‘crime’ will disappear. No sign of a crime can remain if there
is no documentation. You need to have a keen eye to spot scars or bruises on
darker skin.
Description of lesions needs to be metric and repeatable, there
is no reason to not take a photo of a difficult to describe lesion. (although
now there are issues with tampering of photos with programmes such as
photoshop). If you take a picture, place a ruler in the periphery of the lesion
at the same level of the lesion and consider putting a coin in the photo to
help spot distortion or modification of the image later. Lastly make sure you
take the picture perpendicular to the skin surface.
How do you describe a lesion?
Need to address:
- area of body affected
- type of lesion
- colour
- edges/limits
- shape
- orientation
- size
Blunt force trauma
Sharp force trauma
Gun shot wounds
Asphyxia
Thermal injuries
Poisoning
Blunt force trauma
- Excoriations
- Bruising
- Lacerations
Cause by any force against the body surface by a blunt
object. You can tell on a cadaver if the blunt force was performed when the
cadaver was alive or dead by looking at histology. On histology, live tissue injury
will show an inflammatory reaction with extravasation of red blood cells into
the tissue. On dead tissue there is no inflammatory reaction, you can also use
immunohistochemistry to spot the presence of cytokines and see if there are
inflammatory cells present.
Excoriations
Excoriations are loss of the superficial layers of skin due to blunt force
trauma (not an abrasion, an abrasion is loss of the superficial layers of the
skin caused by an object with a sharp margin like a knife). Excoriations often
reproduce the shape of the object that cause it.
Often the excoriation will
heal with a scab and at this point it will become impossible to age the lesion.
ED physicians may be the only people able to preserve material evidence of
assault from the lesion. It’s easy, you simply swab the lesion for 30 seconds
before cleaning the lesion (moisten the
swab with sterile water or saline before), store the swab in a tamper proof
container and dry or freeze it (you can later give it to the police if
necessary). Often under the nails of victim there is often attacker DNA (there
can even be attacker DNA on the surface of a bruise from punches etc).
With excoriations you can often tell in which direction the
blunt injury was caused and this can help reconstruct the event. (yet another
reason for a good description and often there is some material left on the
lesion from whatever object was used to create the lesion).
Scratch marks are a very typical and specific form of
excoriation. Triangular or droplike in shape. They contain a lot of information
about the author of the lesion and genetic information. A tyre mark may be another
kind of distinct lesion (often the actual lesion is caused by the negative
pressure by the treads in the tyre not the actual tyre surface).
Bruising
A bruise means the trauma was in that place, a hematoma is a collection of blood and the trauma causing the hematoma may be elsewhere on the body. When in doubt it is best to describe the lesion as a cutaneous discoloration.
Great example; black eye can be caused by a direct trauma (punch to the face) forming a BRUISE or may be caused by a basilar fracture of the cranium creating the so called racoon eyes this is a HEMATOMA. They will look almost identical.
Note that MRI can be used to age and discover origin of a bruise/hematoma. Not that bruising may be difficult to spot for example of North African darker skin.
A bruise is different to a hematoma!
Bruises are closed lesions that show a distinct
discoloration. The colour relates to the age of the lesion but also the size is
important. You may have different colours at the edge compared to the centre of the lesion due to difference in
breakdown. You need to assess them carefully. For example a patient with multiple small
bruises of same colour you can hypothesise were all caused at the same
time. One large bruise may be purple while a neighbouring small bruise caused
at the same time may be yellow.
Colour therefore depends on physiology, depth of injury and
size.
Remember not to confuse a bruise with a hematoma.
Hematoma = filling of blood into a virtual space
Bruise = forcing of blood into a tissue
Note that old people bruise very easily and may even bruise
spontaneously.
Lacerations
Third kind of blunt injury is a laceration. A laceration is
simply a discontinuation of the skin, you can put the two skin edges together
as normal and reconstruct the skin as there is no loss of substance. Bear in
mind that a skin discontinuation may also be cause by a sharp force trauma. You
have to describe the margins well. Big
clues that the laceration was caused by a blunt force trauma is irregular skin
edges or frayed edges and bridges of tissue. You can look at the subcutaneous tissue
and it will be irregular and not smooth with a blunt force trauma.
Sharp force trauma
- Penetrating injury
- Cut marks
- Stab wounds and mixed injuries
Penetrating injury
Depending on the book you use, pointed objects may or not be
included in this category. A very distinct lesion to look for is needle tracks
or syringe wounds. Always look for syringe marks in any unconscious patient, observe
the whole skin surface, needles may be injected behind the ear or even on the
genitals.
The shape of penetrating object lesions can tell you the
shape of the object tip used to cause the lesion. The flaps of the skin lesions
will match the penetrating object tip for example a squared end will cause an X
shaped flap, a triangular tip will cause a Mercedes sign skin flap and a
circular point a circular lesion.
An example is a penetrating injury to the cranium, surgeons
keep the piece of cranial bone with the penetrating injury, the shape of the
hole in the bone can tell you what kind of object caused the injury.
Cut marks
Cut marks are caused by a sharp edge weapon and cause a neat
discontinuation of the skin edge and tissue. The cut mark usually has a tail at
the edge of the skin discontinuation and this can give you a lot of information
about where pressure was least and hence in what direction the cut was performed
(obviously this depends on the curvature of the skin area and the object used,
its still difficult to tell entry and exit point).
Stab wounds
Mixed weapons can give you stab wounds. These are weapons that can stab and can also cut. The cut mark is the result of passing the sharp edge and
the penetrating injury the result of the pointed edge. Stab wounds contain a
lot of information and will often reproduce the cross section of the blade. For
example a double edged blade will produce a wound with two acute ends, a single
edged blade will produce a wound with a single acute angled corner and an
obtuse angled corner. Sometimes the
going in wound will not match well the going out wound and stab wounds may
crossover each other making the lesion more complex and difficult to describe.
Remember that on skin and bones you may have residues of the
instruments used to cause the lesions and you should always keep any debrided
material.
Gun shot wounds (GSWs)
See future post on gun shot wounds...
Asphyxia
Asphyxia is a manner of death or disease that has distinct signs
left depending on the method of asphyxia, the main types of asphyxia are:
- Smothering
- Choking
- Manual strangulation
- Ligature strangulation
- Hanging
- Drowning
- Traumatic (compression) asphyxia
- Plastic bag suffication
Unfortunately due to frequency of plastic bag suffocations in
forensic pathology it has managed to deserve its own type of asphyxia.
With asphyxia there are many different types lesions that
can be seen on the cadaver such as liver mortis, early rigor, delayed cooling
etc. however, only one type of lesion is found on living bodies, petechiae!
Petechiae
is a very distinct sign of asphyxia and is caused by high pressure in the capillaries
causing them to burst. Not always seen, it can be subtle, for example on the
conjunctiva it is a common sign with strangulation.
Smothering is a good way to get away with murder there is
often no sign apart from petechiae. There may be scratch marks, compression
marks from teeth inside the lips or fibres from the object (usually a pillow).
Choking is usually accidental often people with neurologic
or psychiatric disease or issues with the swallowing reflex.
Strangulation is a mechanism of death and not necessarily the
lack of air. The death can be caused by nervous factors such as compression of
the glomus body of the carotid artery and reflexive cardiac arrest. There are
many anecdotal deaths where an aggressive attacker grabs an old man by the neck
and he just drops dead almost instantly (the attacker will be mentioning in
court how he hardly touched him). You usually see bruising with compression of
the airways. Fracture of the hyoid or cricothyroid cartilage can have a
distinct pattern with strangulation too. A ligature strangulation will often
have a linear bruise of uniform depth sometimes with fibres still around the
area (eg. rope burn).
With hanging there are often distinct fractures and ligature
signs. You can tell easily if the person was hung before or after death by
again looking at the haemorrhaging in the neck and the presence of an
inflammatory response which is lacking with a dead body.
Traumatic asphyxia is caused by a heavy object compressing the
rib cage restricting breathing.
Drowning is an awful way to die, often taking longer than 6
minutes as you alternate between periods of consciousness and unconsciousness. An
important note is that water in the lungs is not proof of drowning! There is
often water in the lungs in cadavers and it may have many origins (although
sometimes it can be obvious with the post autopsy lung able to stand by itself it’s
so full of water). Often the only proof of drowning is the presence of diatoms
(microscopic algae) in the blood and organs (the diatoms being distinct to the
body of water where the drowning occurred). When you drown the alveoli burst
and water mixes with the blood providing an entry point for diatoms to enter
the blood. A long period after drowning
there may be characteristic skin wrinkling and pink discoloration but this is
more for shipwreck victims for example.
Thermal injuries, a common form of abuse. (see post on
burns)
Poisoning
History is so important! Diagnosis of poisoning will
require; anecdotal evidence, autopsy and clinical toxicology. If suspected keep
a sample of blood/urine for a specific toxicology test that may be needed
later. Many poisons are not included in the general toxicology screen performed
in most ER’s. Also consider keeping a small lock of hair (from the roots), with
this you can prove that the drug was not present in the victims system at time
zero.
There were far too many gruesome images that were associated to this post so here is a raccoon reacting to them
Saturday, 5 November 2016
St Emlyn's Emergency Medicine Blog
Shout out to this fantastic blog! Based out of the Manchester Royal Infirmary, St Emlyn's is an emergency medicine blog full of great insights into life as an EM doctor. There are lots of #FOAMed resources for those who are jumping on the social education bandwagon (a more modern version of medical education).
I particularly enjoyed this recent post about the risks of training in EM and why some Dr's quit and how to avoid those lows. @baombejp brings up the following points:
I particularly enjoyed this recent post about the risks of training in EM and why some Dr's quit and how to avoid those lows. @baombejp brings up the following points:
- Dont expect results too fast, take the SMART approach
- Dont fear failure, there are three ways you can react to a setback: you fly, you dive, you thrive
- With regards to the future find the right balance between competence and confidence when progressing and be careful of the unknown'unknowns (the things you dont know you dont know ha)
- Have a life! why have a job if you don't have a life
- There will be ups and downs, find someone to talk to about it
The blog is full of great posts, I enjoyed reading this morning about this consultant dealing with his junior knowing more than him and the following teaching tips.
Labels:
2016,
blog,
emergency,
er,
FOAMed,
life,
lifehacks,
links,
MedED,
medicalblog,
medicalschool,
Medicine
Friday, 4 November 2016
Pulse pressure and atherosclerosis
The pulse pressure is the difference between the systolic blood pressure and the diastolic blood pressure.
PP = SBP -DBP
It is determined by the stroke volume (amount of blood ejected by the heart) and compliance of vessels (the vessels reaction to this bolus of blood).
A higher pulse pressure will be measured in the smaller arteries further from the heart, as the pressure drops and the compliance increases.
Elderly patients that have stiffer vessels with a lower compliance will have a higher pulse pressure, but this isn't the whole story. The pressure wave reflects along the vessels and is reflected more easily by a very stiff vessel (harder vessel has less give, so wave travels faster, less delay, a high pulse wave velocity). Usually the wave reflects and returns during the diastolic phase but when the wave returns earlier it can increase the measured systolic pressure and lower the measured diastolic pressure, overall increasing the pulse pressure. (picture below describes this much better graphically).
PP can be considered an independent prognostic factor for cardiovascular morbidity (and it makes sense as a sort of crude marker of atherosclerosis and arterial stiffness).
Higher PP is proven to be related to smoking, diabetes, dyslipidemia, obesity and power sports activity.
Every 10mmHg increase in PP is associated with an increase in cardiovascular death risk of around 10%. However, also a low PP (below 45mmHg in patients with already advanced heart disease is linked with increased mortaility).
Wide PP for example >80mmHg is almost diagnostic in the case of severe aortic regurgitation.
The value to look for is a peripheral PP over 55-60 mmHg, this should alert you to likelihood of arterial stiffness and increased cardiovascular risk.
PP = SBP -DBP
It is determined by the stroke volume (amount of blood ejected by the heart) and compliance of vessels (the vessels reaction to this bolus of blood).
A higher pulse pressure will be measured in the smaller arteries further from the heart, as the pressure drops and the compliance increases.
Elderly patients that have stiffer vessels with a lower compliance will have a higher pulse pressure, but this isn't the whole story. The pressure wave reflects along the vessels and is reflected more easily by a very stiff vessel (harder vessel has less give, so wave travels faster, less delay, a high pulse wave velocity). Usually the wave reflects and returns during the diastolic phase but when the wave returns earlier it can increase the measured systolic pressure and lower the measured diastolic pressure, overall increasing the pulse pressure. (picture below describes this much better graphically).
PP can be considered an independent prognostic factor for cardiovascular morbidity (and it makes sense as a sort of crude marker of atherosclerosis and arterial stiffness).
Higher PP is proven to be related to smoking, diabetes, dyslipidemia, obesity and power sports activity.
Every 10mmHg increase in PP is associated with an increase in cardiovascular death risk of around 10%. However, also a low PP (below 45mmHg in patients with already advanced heart disease is linked with increased mortaility).
Wide PP for example >80mmHg is almost diagnostic in the case of severe aortic regurgitation.
The value to look for is a peripheral PP over 55-60 mmHg, this should alert you to likelihood of arterial stiffness and increased cardiovascular risk.
Tuesday, 1 November 2016
Subscribe to:
Comments (Atom)